Ruth A. Etzel, MD, PhD (USA) – Chair - [email protected]
Jie Ding, MD, PhD (China)
Stella M. Gil, MD (Argentina)
David Githanga, MD, PhD (Kenya)
Alok Gupta, MD (India)
Salman Mroueh, MD (Lebanon)
Environmental Health Advocates from National Pediatric Societies:
Dr. Abdullah Al-Omair (Saudi Arabia)
Dr. Olga Cirstea (Moldova)
Dr. Lydiana Avila De Benedictis (Costa Rica)
Dr. Immaculate K-Barasa (Kenya)
Dr. Alvin S. M. Chang (Singapore)
Dr. Juan Antonio Ortega Garcia (Spain)
Dr. Rose A. Kambarami (Zimbabwe)
Dr. Selva Kumar Sivapunniam (Malaysia)
Dr. Peter Le Souef (Australia)
Dr. Damian Nwaneri (Nigeria)
The Strategic Advisory Group began as the Technical Advisory Group, initiated by the Standing Committee of the International Pediatric Association (IPA) in 2001. Under the leadership of Dr. Ruth Etzel, Chair of the Technical Advisory Group, in 2005 the IPA launched the International Pediatric Environmental Health Leadership Institute to better prepare the world’s pediatricians to address environmental health issues. The Institute was funded by a $150,000 grant to IPA from the U.S. Environmental Protection Agency. IPA sponsored one-day Environmental Health Workshops in 2005, 2007, 2010, 2013 and 2016 to fulfill the needs of pediatricians wishing to learn more about child health and the environment. Pediatricians who successfully completed the workshop and passed an examination were accepted into the International Pediatric Environmental Health Leadership Institute.
A growing number of diseases in children from rural and urban areas are linked to unsafe, degraded environments. However, many health care providers are unable to recognize, assess and manage environmentally-related diseases in children.
How should this problem be addressed?
Enabling those "in the front line" - the health professionals dealing with children and adolescent's health- to recognize and assess diseases linked to, or triggered by environmental factors. Paediatricians, family doctors, nurses, primary and other health care workers should be trained on the relationships between children's health and the environment through the use of harmonized training materials, adaptable to the specific needs of countries and professional groups.
What are the benefits of training health care providers?
Increased understanding about the influence of environmental factors on children's health
Improved quality of diagnosis and management of environmentally-related health and developmental effects
Capacity to discuss environmental risks with patients, parents, educators and the media
Advocacy skills for sensitizing decision-makers about high priority issues for action
Enhanced potential for research on children's health
What is the WHO Training Package for Health Care Providers?
A collection of over 30 modules with internationally harmonized information and peer-reviewed materials to enable health care workers to be trained, and also to become trainers of their peers and colleagues. The modules include extensive notes and references, case studies and self-evaluation tools, backed up by manuals and guidelines. A selected team of experienced professionals from over 15 countries, the International Paediatric Association (IPA) and selected NGOs are participating in its preparation.
This initiative was made possible thanks to the financial support provided by the US EPA Office of Children's Health Protection, that also made available useful data, graphics and text for the modules.
What issues are covered?
The special vulnerability of children to physical, chemical and biological environmental threats
The health and developmental effects of specific chemical, physical and biological hazards (e.g. pesticides, persistent toxic pollutants -POPs- , lead, arsenic, radiation, noise, moulds, other) present in specific settings (e.g. home and surroundings, school, recreation areas, workplace, fields, other)
Sources, routes and mechanisms of exposure (contaminants in air, water, food, cosmetics, objects, toys, medical devices, that may be inhaled, ingested or absorbed...)
Illustrative case studies.
How are the training programmes organized and by whom?
Training events are organized according to the needs identified by the countries and/or scientific groups concerned and financial resources available. WHO provides technical advice on the contents and methodology. The event may go from a 1-day introductory course to a full 40-hour course that enables to cover the entire contents of the package. WHO and its partners provide the initial training and distribution of materials, some of which are available as informal versions in Spanish, French and Russian thanks to the contribution of partners in different countries.
1. Why children
2. Children are not little adults
3. Indoor air pollution
4. Outdoor air pollution
5. Lead
6. Mercury
7. Pesticides
8. POPs
9. Water
10. Paediatric environmental history
11. Cancer
12. Food safety
13. Global climate change
14. Injuries
15. Noise
16. Occupational exposure
17. Radiation
18. Respiratory diseases
19. Children's Environmental
20. Second-hand tobacco smoke and children
21. Mycotoxins.
22. Children and chemicals.
23. Biomarkers and human biomonitoring.
24. Immune diseases and children.
25. Developmental and environmental origins of adult disease.
26. Children & neurodevelopmental disorders.
27. Endocrine disorders.
28. Sanitation and hygiene.
29. Children and other heavy metals.
A. Participate in meetings of the WHO-Civil Society Working Group on Climate and Health
The Strategic Advisory Group will provide input through the Working Group to the WHO report to the UN Framework Convention on Climate Change (UNFCCC) for the climate negotiation process at the UN Climate Conference in Scotland in November 2021 (COP26).
B. Collaborate with the International Society for Social Pediatrics and Child Health to provide a series of webinars on climate change and child health
This series of 8 webinars discussed how pediatricians and child health providers can and should respond to the climate crisis. The webinars were held monthly from March to September of 2021. Dr. Ruth Etzel, the Chair of the IPA Strategic Advisory Group presented the Declaration on Climate Change at the second webinar on March 25, 2021.
C. Assist National Pediatric Societies with tracking selected SDG indicators on Environmental Health
The following 4 sustainable development goals (SDGs) will be tracked because of their importance to child health in all countries:
1. Urban air pollution (SDG Indicator 11.6.2)
2. Access to clean fuels for cooking (SDG Indicator 7.1.2)
3. Safe drinking water (SDG Indicator 6.1.1)
4. Integration of climate change into national policies (SDG Indicator 13.2.1)
D. Continue the International Pediatric Environmental Health Leadership Institute
A 6-hour Environmental Health workshop is planned for the next Congress of Pediatrics.
E. Participate in Global Lead Paint Alliance
The Strategic Advisory Group will continue to participate with WHO and UNEP in the Global Lead Paint Alliance, as it has done since 2013. This Alliance works to end the use of lead paint around the world. Each October the Strategic Advisory Group shares customizable outreach materials with pediatric organizations for national awareness days for prevention of lead poisoning with an emphasis on the risks of lead paint.
F. IPA İhsan Doğramaci Prize in Children's Environmental Health
The Prize will be widely advertized to enable the IPA to identify a possible recipient to be awarded at the next Congress of Pediatrics.
Urban air pollution
SDG Indicator 11.6.2
Definition: Indicator 11.6.2 is the annual mean levels of fine particulate matter (e.g. PM2.5 and PM10) in cities (population weighted).
This indicator measures the population-weighted exposure to ambient PM2.5 pollution; that is, concentrations of suspended particles measuring less than 2.5 microns in diameter.
Goal: By 2030, reduce the adverse per capita environmental impact of cities, including by paying special attention to air pollution.
Access to clean fuels for cooking
SDG Indicator 7.1.2
Definition: Indicator 7.1.2 is the proportion of population with primary reliance on clean fuels and technology.
This is measured as the share of the total population with access to clean fuels and technologies for cooking. Access to clean fuels or technologies such as clean cookstoves reduce exposure to indoor air pollutants, a leading cause of death in low-income households.
Goal: By 2030 ensure universal access to affordable, reliable and modern energy services.
Safe drinking water
SDG Indicator 6.1.1
Definition: Indicator 6.1.1 is the proportion of population using safely managed drinking water services.
A safely managed drinking water service is defined as one located on premises, available when needed and free from contamination.
Goal: By 2030 achieve universal and equitable access to safe and affordable drinking water for all.
Integration of climate change into national policies
SDG Indicator 13.2.1
Definition: Indicator 13.2.1 is the number of countries that have communicated the establishment or operationalization of an integrated policy/strategy/plan which increases
their ability to adapt to the adverse impacts of climate change and foster climate resilience and low greenhouse gas emissions development.
This indicator measures the number of countries signed on to multilateral agreements on climate change. Currently this indicator does not reflect the levels of operationalization or implementation of climate mitigation and adaption action.
National commitments within the UNFCCC Paris Agreement vary by country depending on their Nationally Determined Contributions (NCDs) so are not directly comparable. In the additional charts below you will find data on national CO2 emissions, per capita emissions and carbon intensity measures.
Goal: By 2030 integrate climate change measures into national policies, strategies and planning.
click here to download Workshop Registration Form - Vancouver, August 17, 2016
click here to download Pre Congress Environmental Health Workshop, Vancouver, August 17, 2016
click here to view Report of the Summit on Child Health and the Environment 2014
In 2015, 5.9 million children under age five died. The major causes of child deaths globally are pneumonia, prematurity, intrapartum-related complications, neonatal sepsis, congenital anomalies, diarrhoea, injuries and malaria. Most of these diseases and conditions are at least partially caused by the environment. It was estimated in 2012 that 26% of childhood deaths and 25% of the total disease burden in children under five could be prevented through the reduction of environmental risks such as air pollution, unsafe water, sanitation and inadequate hygiene or chemicals.
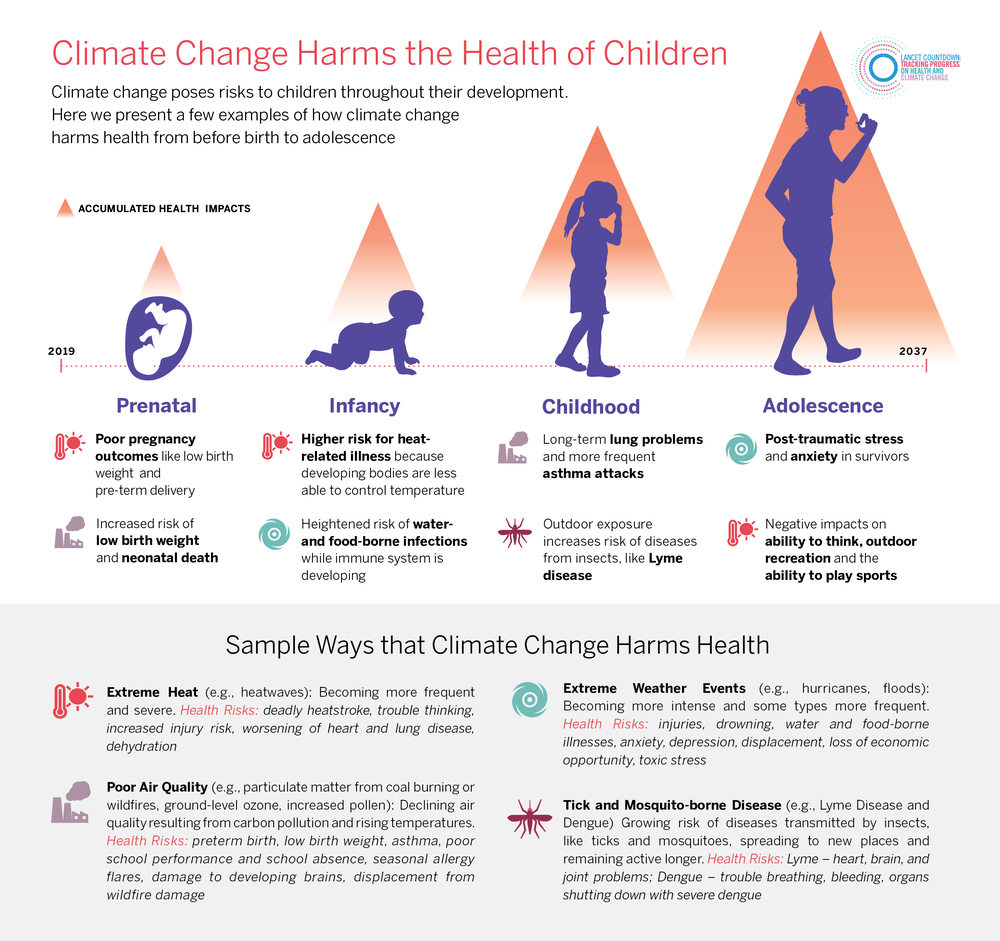
Children are especially vulnerable to environmental threats due to their developing organs and immune systems, smaller bodies and airways. Harmful exposures can start as early as in utero. Furthermore, breastfeeding can be an important source of exposure to certain chemicals in infants; this should, however, not discourage breastfeeding which carries numerous positive health and developmental effects (4). Proportionate to their size, children ingest more food, drink more water and breathe more air than adults. Additionally, certain modes of behaviour, such as putting hands and objects into the mouth and playing outdoors can increase children’s exposure to environmental contaminants.
Don’t pollute my future! The impact of the environment on children’s health.
Program activities
Environmental Health Committee Goals/Objectives for 2011:
Continue to Develop the Pediatric Environmental Health Leadership Institute
Goal/Objective 1: Put Children's Environmental Health Training Modules on the IPA website and advertise to pediatricians worldwide
Goal/Objective 2: In collaboration with at least 3 National Pediatric Societies, conduct workshops to train pediatricians in children's environmental health and improve their capacities for leadership in the recognition, diagnosis, prevention and management of pediatric diseases linked to environmental factors and enable them to offer advice and information to policymakers in their communities. Consider holding workshop in Mumbai, India in conjunction with the 14th World Conference on Tobacco or Health in March, 2009
Goal/Objective 3: Standardize, evaluate and ensure the competence level of pediatricians in children�s environmental health through an international credentialing program that will be implemented in coordination with National Pediatric Societies.
Goal /Objective 4: Facilitate global communications, networking and exchange of ideas among pediatricians on prevention and treatment of childhood illnesses linked to the environment.
Goal/Objective 5: Write a manuscript for the peer-reviewed literature summarizing the progress in developing the Pediatric Environmental Health Leadership Institute
Goal/Objective 6: Write a grant to support the development of a rapid response team of pediatricians with specific training who could respond to requests from the World Health Organization and other organizations when environmental disasters occur and a pediatrician�s advice is needed.
Goal/Objective 7: Work with other organizations towards the elimination of tobacco from homes with children and the elimination of lead from petrol.
IPA Statements and publications
- IPA Report of 4 August 2010 Pre-Conference Workshop for Pediatricians Johannesburg
- IPA Statement on Second hand smoke and Children
- Nairobi Declaration
- IPA Statement on Pediatric Environmental Health Specialty Centres
- IPA Statement on Tobacco
- Workshop on Children's Health and the Environment, Athens, Greece August 25, 2007
- Workshop on Children's Health and the Environment, Port-au-Prince, Ha�ti, June 3-6, 2007
- Workshop on Children's Health and the Environment, New Delhi, India, February 23-25, 2007
- Workshop on Children's Health and the Environment, Nairobi, Kenya, October 12-14, 2005
- Dr. Ruth A. Etzel, IPA Technical Advisor in Children's Environmental Health, named 2007 Children's Environmental Health Champion by the United States Environmental Protection Agency�s Office of Children's Health Protection
Awards
Click here to Read
Recent publications about Children's Health and the Environment
Children's Exposure to Mercury Compounds
Healthy Environments for Healthy Children
Children's Environmental Health Units
Persistent Organic Pollutants: Impact on Child Health
Educational Leaflets
Click here to zoom image
Research Findings 2017
1) August 2017 click here
2) July 2017 click here
3) May 2017 click here
4) April 2017 click here
5) March 2017 click here
Research Findings 2016
1) July 2016 click here
2) June 2016 click here
3) May 2016 click here
4) March 2016 click here
5) February 2016 click here
6) January 2016 click here
Research Findings 2015
1) December 2015 click here
2) November 2015 click here
3) October 2015 click here
4) September 2015 click here
5) August 2015 click here
6) July 2015 click here
7) June 2015 click here
8) May 2015 click here
9) April 2015 click here
10) March 2015 click here
11) February 2015 click here
12) January 2015 click here
Research Findings 2014
1) December 2014 click here